Endodontic Treatment Chula Vista, CA
Who performs endodontic treatment?
All dentists, including your general dentist, received training in endodontic treatment in dental school. General dentists can perform endodontic procedures along with other dental procedures, but often they refer patients needing endodontic treatment to endodontists.
Endodontists are dentists with special training in endodontic procedures. They provide only endodontic services in their practices because they are specialists. To become specialists, they complete dental school and an additional two or more years of advanced training in endodontics. They perform routine as well as difficult and very complex endodontic procedures, including endodontic surgery. Endodontists are also experienced at finding the cause of oral and facial pain that has been difficult to diagnose.
What is endodontic treatment?
 “Endo” is the Greek word for “inside” and “odont” is Greek for “tooth.” Endodontic treatment involves the inside of the tooth.
“Endo” is the Greek word for “inside” and “odont” is Greek for “tooth.” Endodontic treatment involves the inside of the tooth.
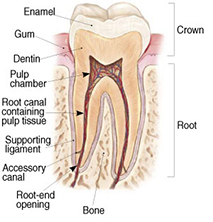
To understand endodontic treatment, it helps to know something about the anatomy of the tooth. Inside the tooth, under the white enamel and a hard layer called the dentin, is a soft tissue called the pulp. The pulp contains blood vessels, nerves and connective tissue, and creates the surrounding hard tissues of the tooth during development.
The pulp extends from the crown of the tooth to the tip of the roots where it connects to the tissues surrounding the root. The pulp is important during a tooth’s growth and development. However, once a tooth is fully mature it can survive without the pulp, because the tooth continues to be nourished by the tissues surrounding it.
Why would I need endodontic treatment?
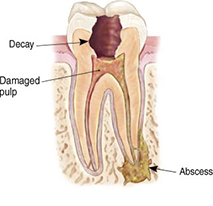
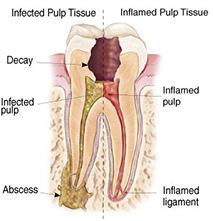 Endodontic treatment is necessary when the pulp becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, repeated dental procedures on the tooth, faulty crowns, or a crack or chip in the tooth. In addition, trauma to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
Endodontic treatment is necessary when the pulp becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, repeated dental procedures on the tooth, faulty crowns, or a crack or chip in the tooth. In addition, trauma to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
Signs of pulp damage include pain, prolonged sensitivity to heat or cold, discoloration of the tooth, and swelling and tenderness in the nearby gums. Sometimes, there are no symptoms.
How does endodontic treatment save the tooth?
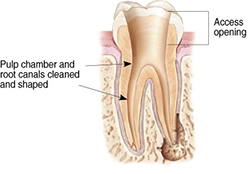
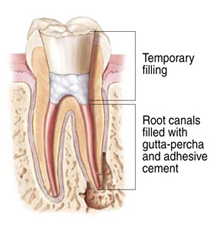
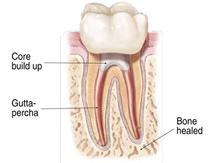
The endodontist removes the inflamed or infected pulp, carefully cleans and shapes the inside of the tooth, then fills and seals the space. Afterwords, you will return to your dentist, who will place a crown or other restoration on the tooth to protect and restore it to full function.
Will I feel pain during or after the procedure?
Many root canal procedures are performed to relieve the pain of toothaches caused by pulp inflammation or infection. With modern techniques and anesthetics, most patients report that they are pain-free during the procedure.
For the first few days after treatment, your tooth may feel sensitive, especially if there was pain or infection before the procedure. This discomfort can be relieved with over-the-counter or prescription medications. Follow Dr. Massarat’s instructions carefully.
Your tooth may continue to feel slightly different from your other teeth for some time after your endodontic treatment is completed. However, if you have severe pain or pressure or pain that lasts more than a few days, call our office.
Endodontic Procedure
Endodontic treatment can often be performed in one or two visits and involves the following steps:
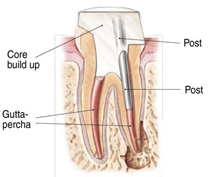
If the tooth lacks sufficient structure to hold the restoration in place, your dentist or endodontist may place a post inside the tooth. Ask your dentist or endodontist for more details about the specific restoration planned for your tooth.
How much will the procedure cost?
The cost varies depending on how complex the problem is and which tooth is affected. Molars are more difficult to treat, so the fee is usually more. Most dental insurance policies provide some coverage for endodontic treatment.
Generally, root canal treatment and restoration of the natural tooth are less expensive than the alternative of having the tooth extracted. An extracted tooth must be replaced with a bridge or implant to restore chewing function and prevent adjacent teeth from shifting. These procedures tend to cost more than endodontic (root canal) treatment and appropriate restoration. With root canal treatment you save your natural teeth and money.
Will the tooth need any special care or additional treatment?
You should not chew or bite on the treated tooth until you have had it restored by your regular dentist. The unrestored tooth is susceptible to fracture, so you should see your regular dentist for a full restoration as soon as possible. Otherwise, you need only practice good oral hygiene, including brushing, flossing, and regular checkups and cleanings.
Most root canal treated teeth last as long as other natural teeth. In a few cases, a tooth that has undergone endodontic (root canal) treatment does not heal or the pain continues. Occasionally, the tooth may become painful or diseased months or even years after successful treatment. Often when this occurs, redoing the endodontic procedure can save the tooth.
What causes a root canal treated tooth to need additional treatment?
New trauma, deep decay, or a loose, cracked or broken filling can cause new infection in your tooth. In some cases, Dr. Massarat may discover additional very narrow or curved canals that could not be treated during the initial procedure.
Can all teeth be treated endodontically?
Most teeth can be treated. Occasionally, a tooth can’t be saved because the root canals are not accessible, the root is severely fractured, the tooth doesn’t have adequate bone support, or the tooth cannot be restored. However, advances in root canal treatment are making it possible to save teeth that even a few years ago would have been lost. When root canal treatment is not effective, endodontic surgery may be able to save the tooth.
What is endodontic surgery?
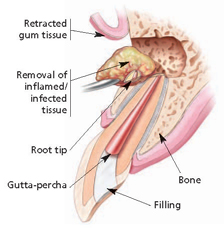 The most common endodontic surgical procedure is called an apicoectomy or root-end resection. When inflammation or infection persists in the bony area around the end of your tooth after endodontic treatment, your endodontist may perform an apicoectomy. In this procedure, the endodontist opens the gum tissue near the tooth to expose the underlying bone, and the infected tissue is removed. The very end of the root is also removed, and a small filling may be placed to seal the root canal. Local anesthetics make the procedure comfortable, and most patients return to their normal activities the next day.
The most common endodontic surgical procedure is called an apicoectomy or root-end resection. When inflammation or infection persists in the bony area around the end of your tooth after endodontic treatment, your endodontist may perform an apicoectomy. In this procedure, the endodontist opens the gum tissue near the tooth to expose the underlying bone, and the infected tissue is removed. The very end of the root is also removed, and a small filling may be placed to seal the root canal. Local anesthetics make the procedure comfortable, and most patients return to their normal activities the next day.
What are the alternatives to endodontic treatment?
When the pulp of a tooth is damaged, the only alternative to endodontic treatment is extraction of the tooth. To restore chewing function and to prevent adjacent teeth from shifting, the extracted tooth must be replaced with an implant or bridge. This requires surgery or dental procedures on adjacent healthy teeth and can be far more costly and time-consuming than endodontic treatment and restoration of the natural tooth.
No matter how effective modern tooth replacements are – and the can be very effective – nothing is as good as a natural tooth.




